How to support nurses to provide palliative care in hospitals to benefit both nurses’ and patients’ well-being?
--- Palliative terminal care VR training for inexperienced nurses on emotional and spiritual capability
/Project info
Project length: 2month research + 2month design
Project type: Individual work
Skills: Design research, creative facilitation (online), visualization, rapid-prototyping, user test&iteration, VR demo making
#Experience/Service design
#Design for healthcare professionals’ wellbeing
#Holistic research strategy
#VR learning
#Remote stakeholder management
/Project Overview
Collaborated with Maasstad Hospital (Rotterdam, NL) and End of Life Lab (TU Delft), this project aims to investigate how to support nurses in the Oncology Department of Maasstad Hospital to be able to provide palliative care to patients.
There is a lack of specialized palliative care education and training in nursing schools as well as in hospitals. If beginning nurses are assigned to dying patients, they can only learn from practice or peers. The quick working pace leaves them little time to digest and reflect everything they’ve experienced or learned. These factors drive them away from the opportunity at the beginning of their career to form the skills of how to cope with death, dying patients and their loved ones, causing mental stress and reducing the care quality for the patients.
The design aims to support junior nurses with palliative care on-site learning, creating virtual training application of palliative care for inexperienced nurses on emotional and spiritual capabilities, where nurses gradually become mentally prepared to provide palliative terminal care for dying patients and families through own explorations and reflections, to ensure nurses’ mental well-being while being able to provide emotional and spiritual care to patients and families with quality.
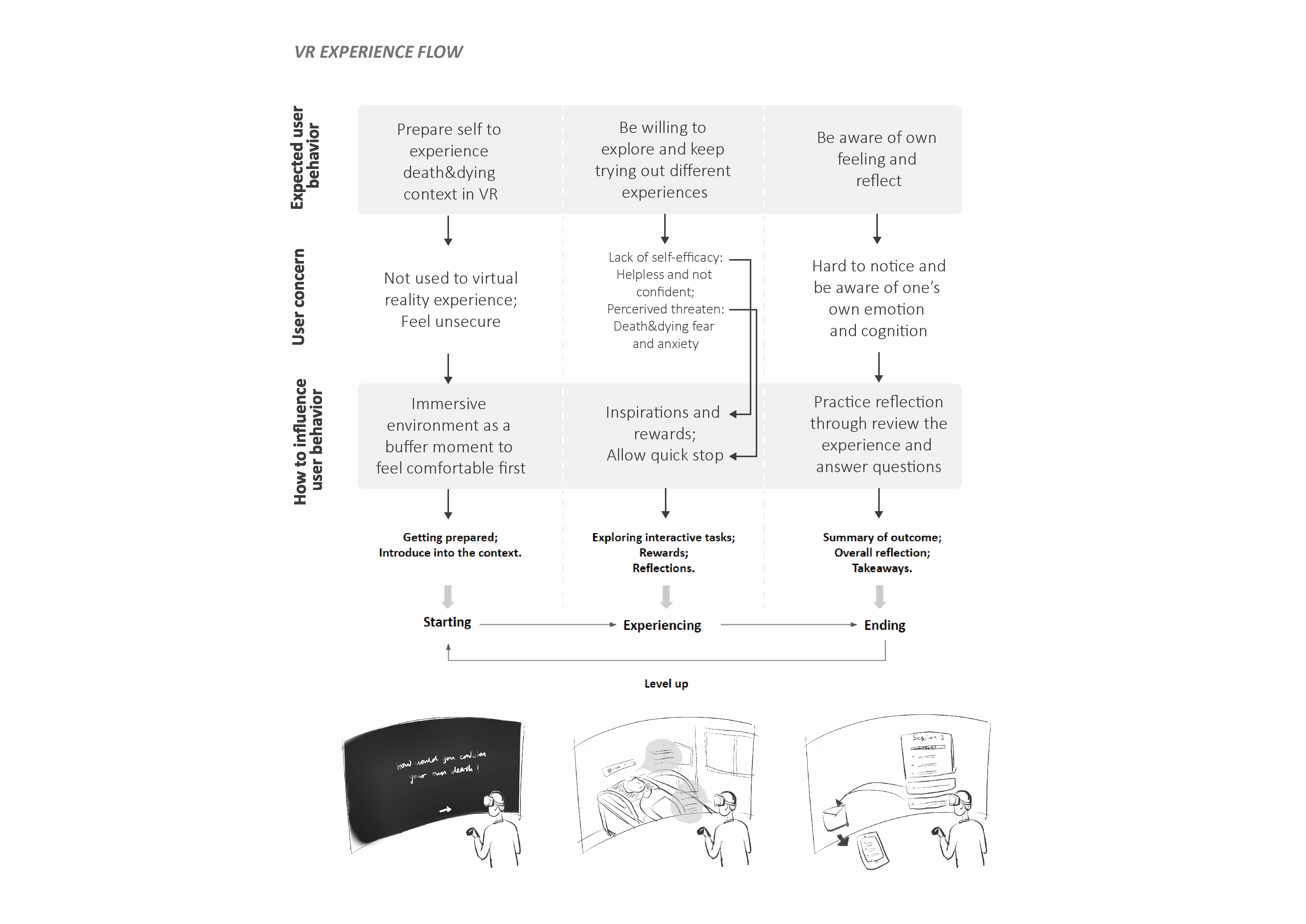
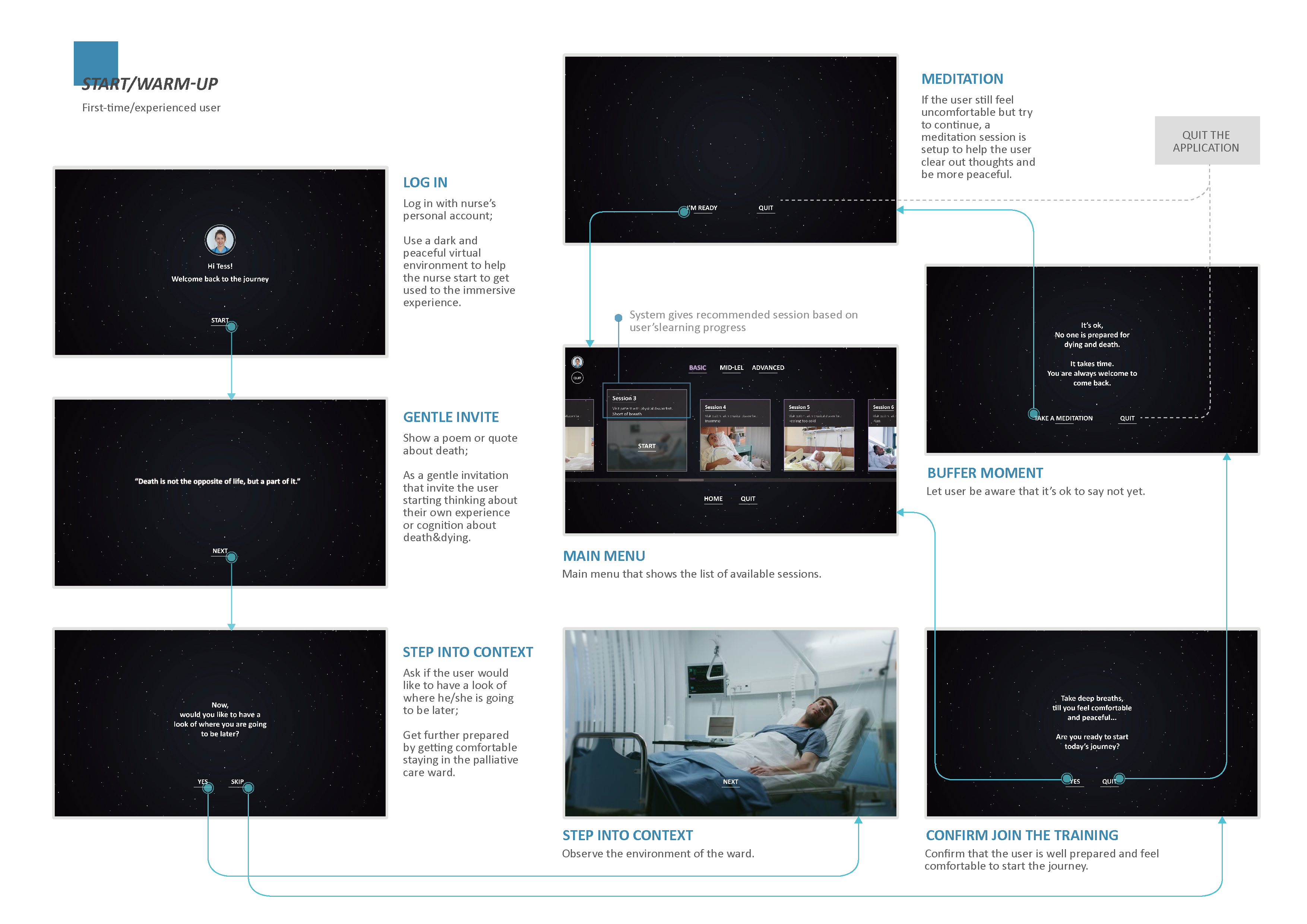
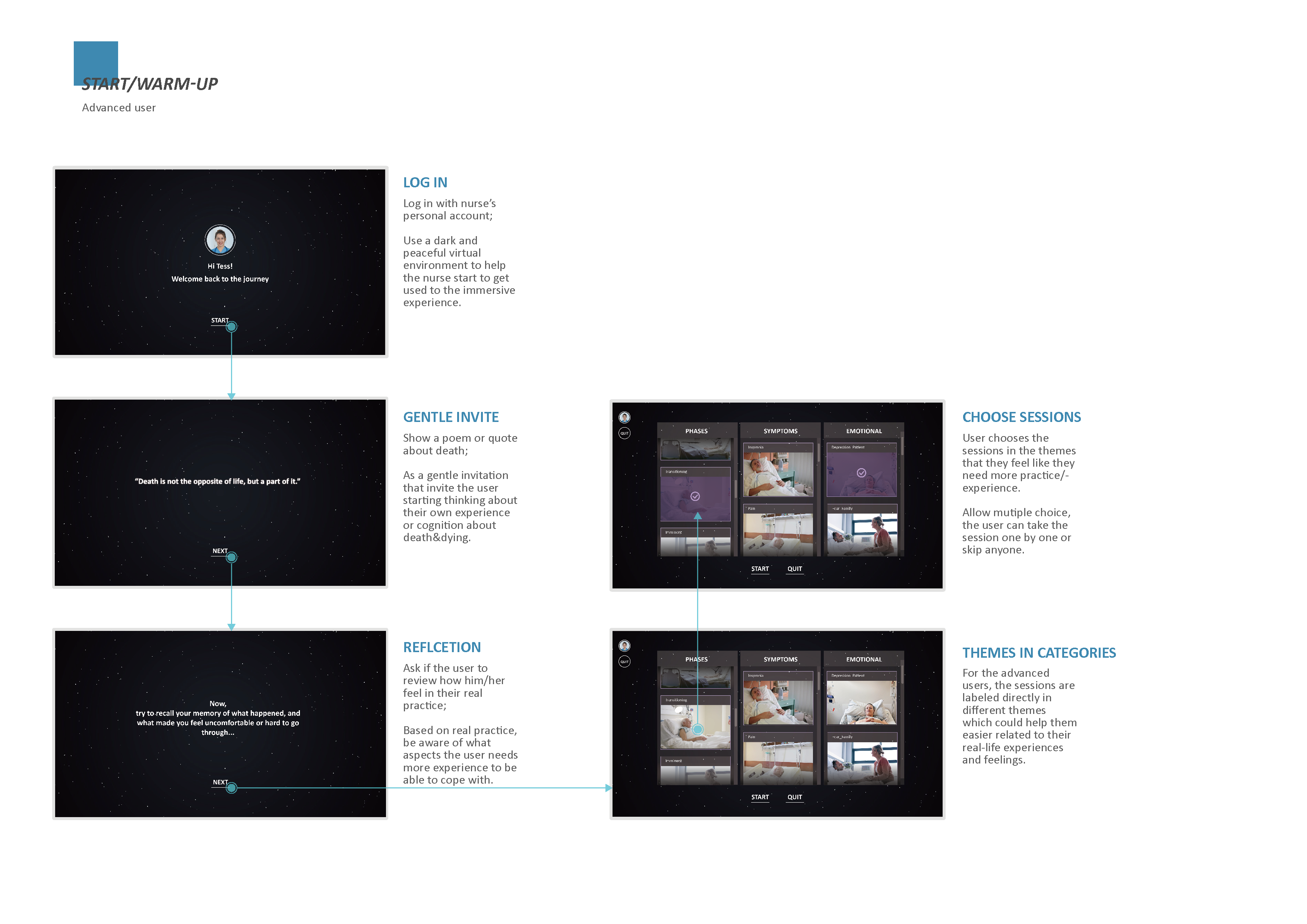
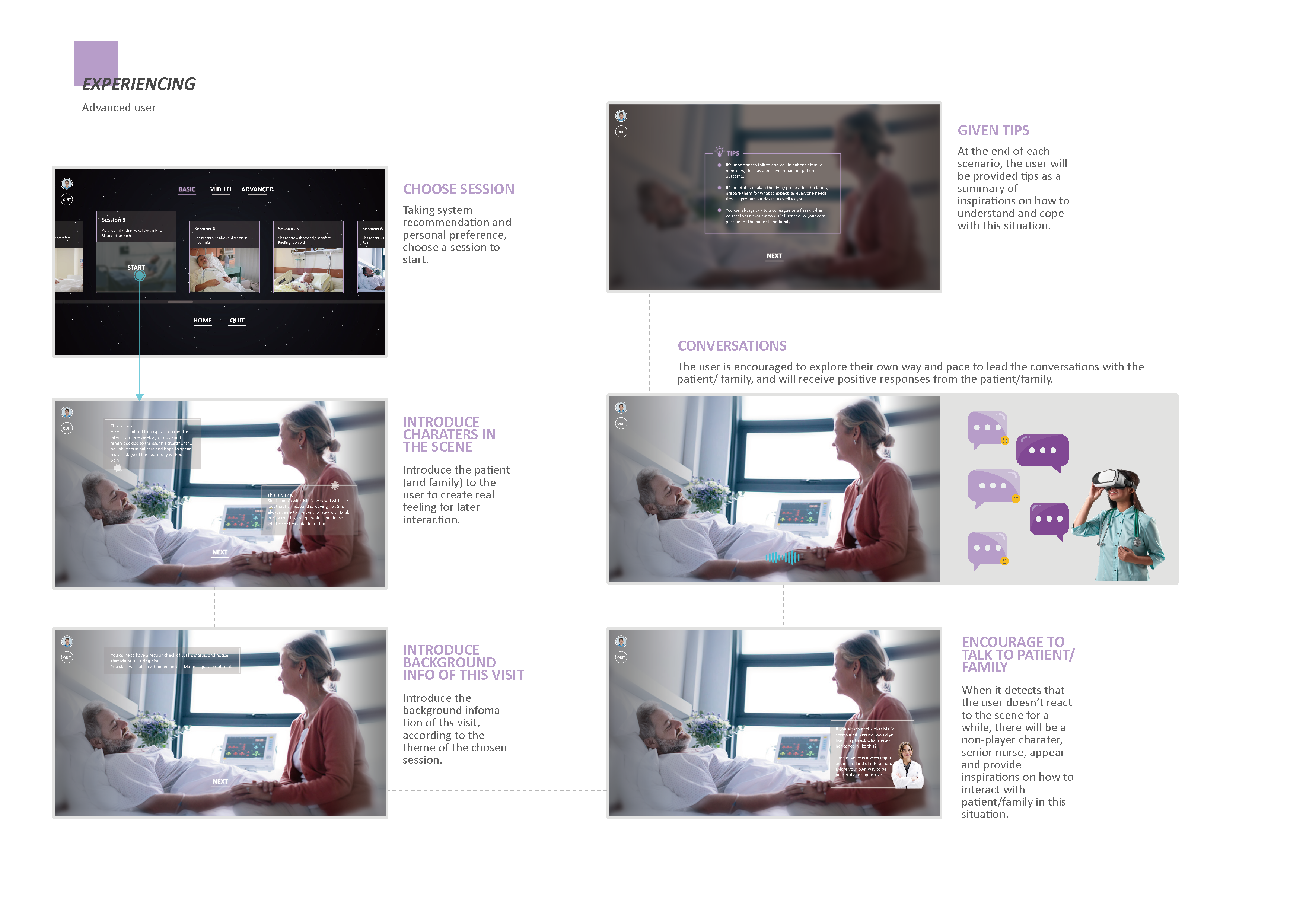
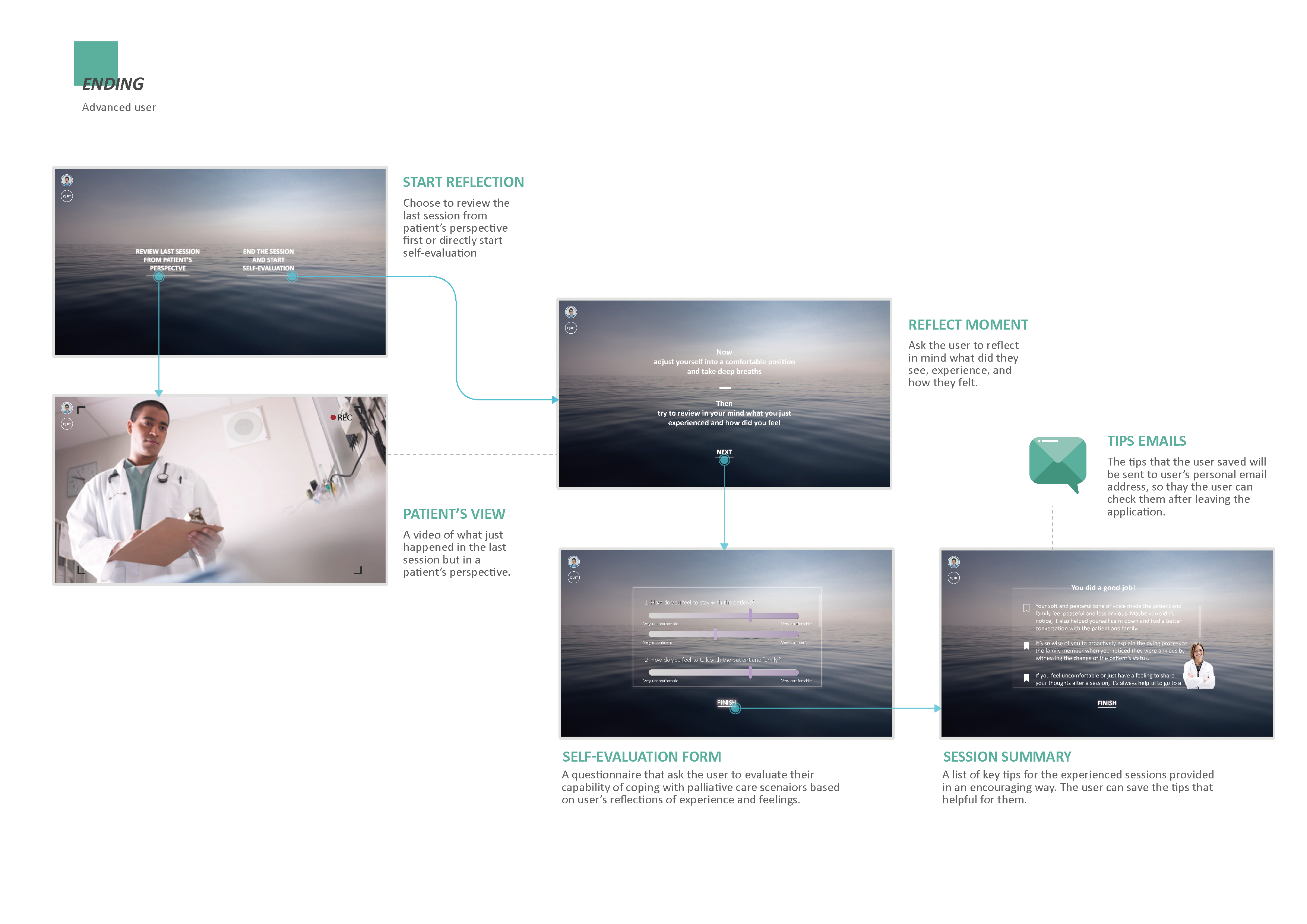
/Experience of a single training session
Several user scenarios are created to demonstrate how this application helps the users get on board and get inspired, as well as allow the users feel as comfortable as possible while using it:
The final design, which is made into a VR demo, is perceived by the nurse as to be promising to provide the inexperienced nurses or even other medical professionals with a safe environment to learn to cope with their own feelings, explore and make mistakes, and be eventually more comfortable and confident to look after dying patients and their family members.
The detailed concept system is elaborated in the map shown in the figure below. It explains how the service supports the contents of the VR training application, as well as how the VR application supports forming the user experience journey.
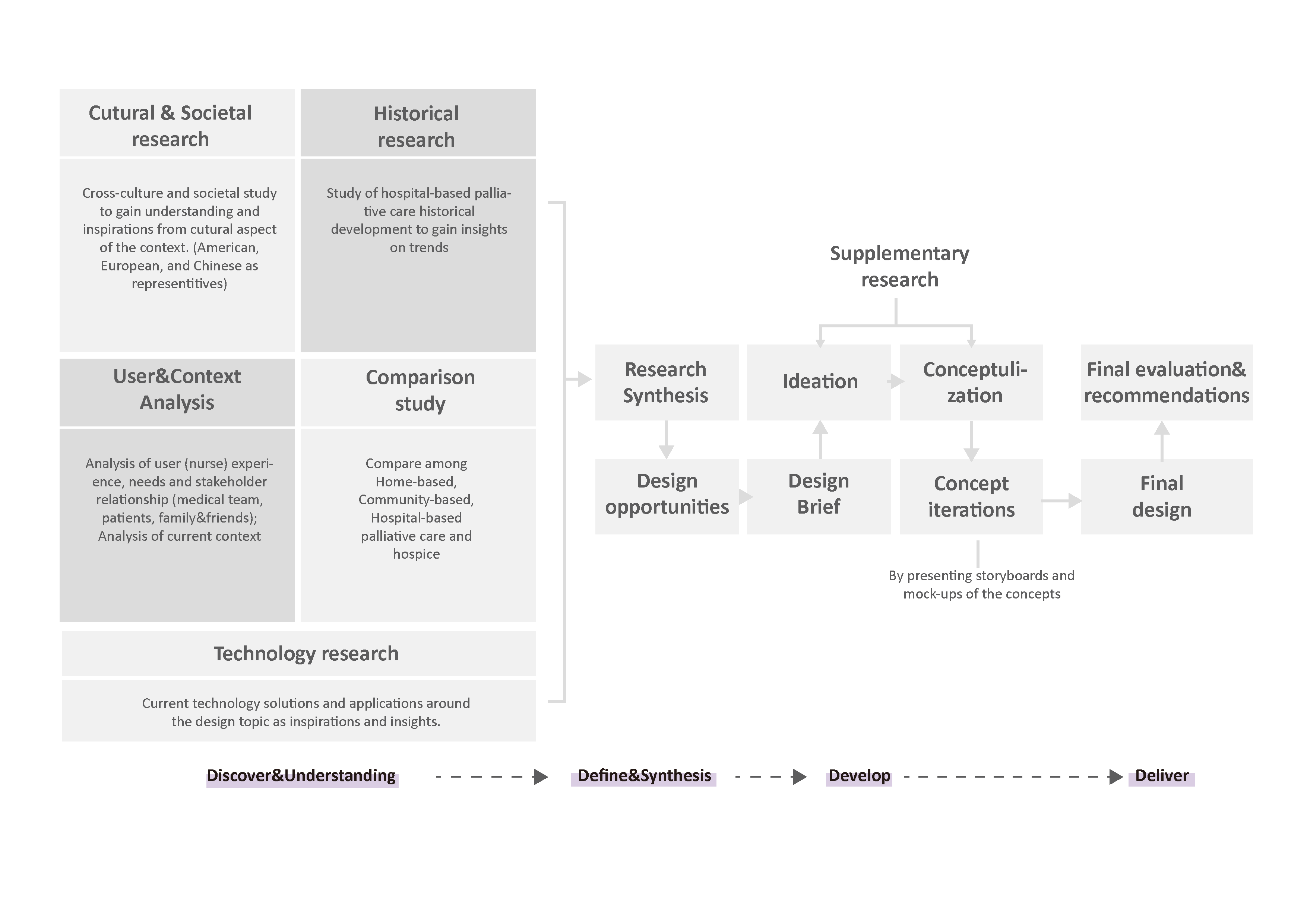
/Project Approach
/Design Development and Elaboration
1. Research insights
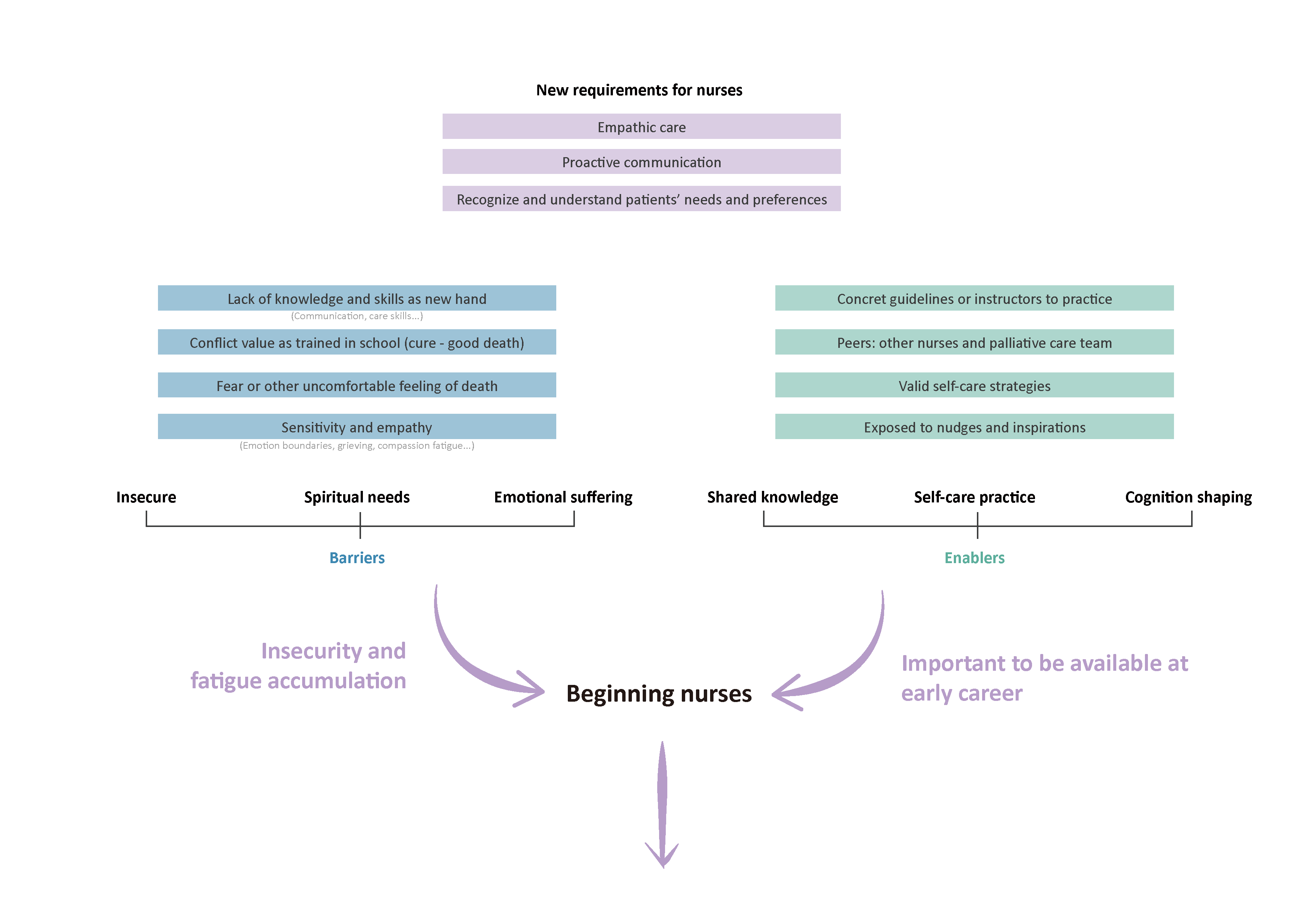
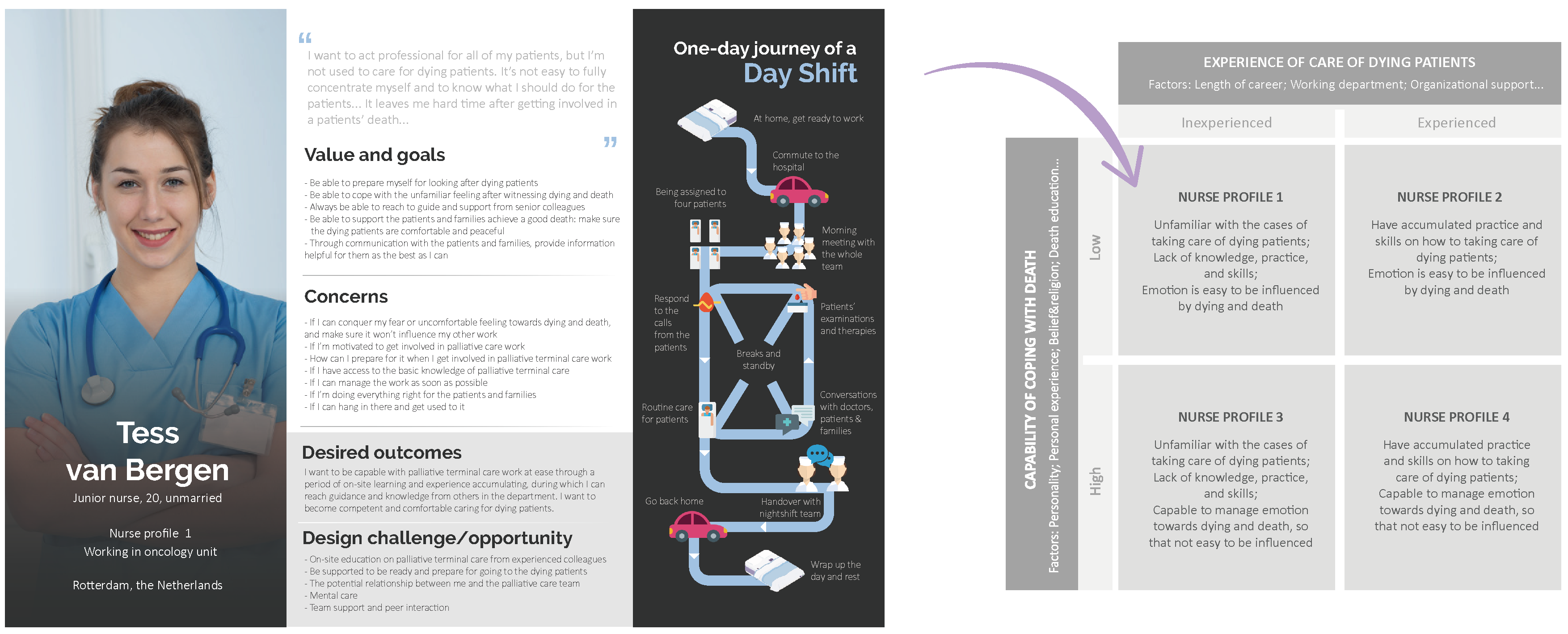
In general, the palliative-care-inexperienced nurtises are lack of specialized education and training on palliative terminal care, as well as lack of time in their fast pace of work to cope with their own experience and emotions, while the patient&family are in need of physical&social&emotional&spiritual support and expecting their needs can be recognized and supported by nurses.
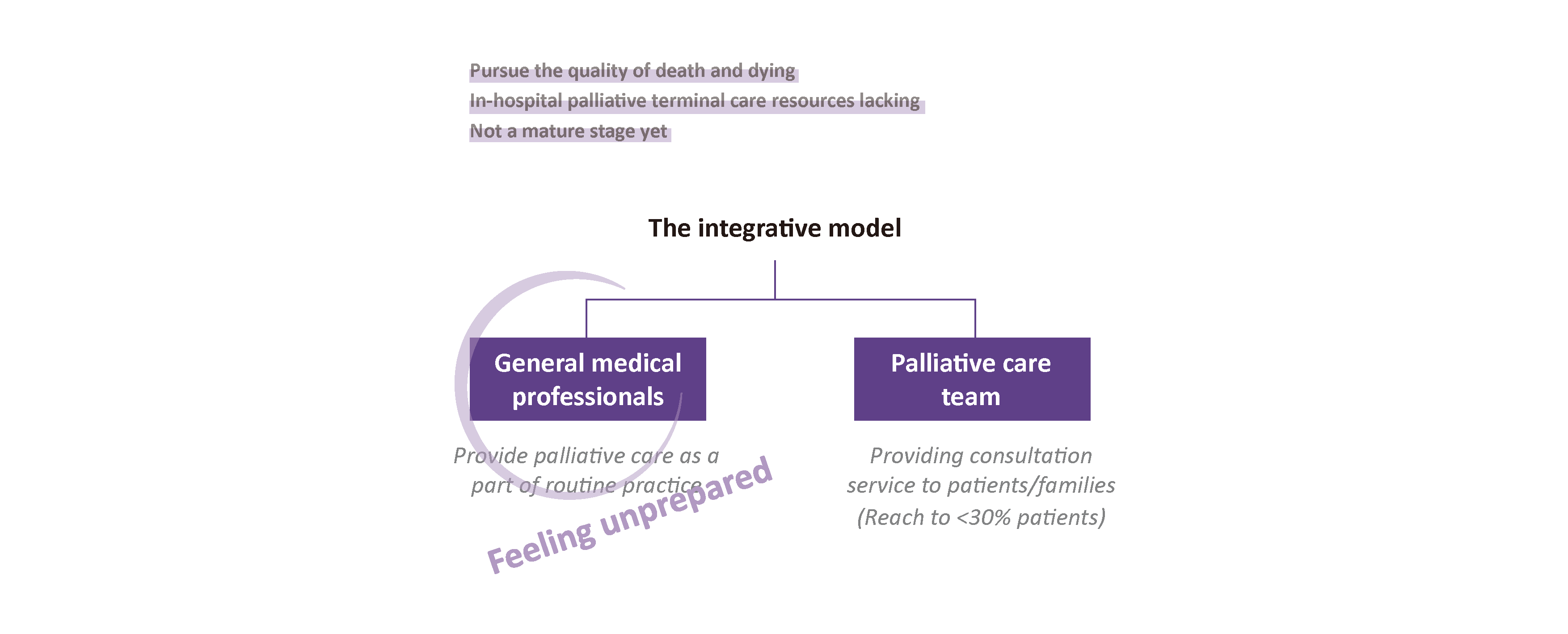
Problem of current model of in-hospital palliative care setting:
Barriers and enablers:
Go to research elaboration ︎︎︎
2. Design goal
“How to enable on-site learning for junior and inexperienced nurses to cope with providing care to dying patients?”
After mapping out potential solution directions (Go to more discussed directions︎︎︎), discussing with stakeholders from Maasstad Hospital, and making the design decision, the project in the following design phase will focus on solving the question below:
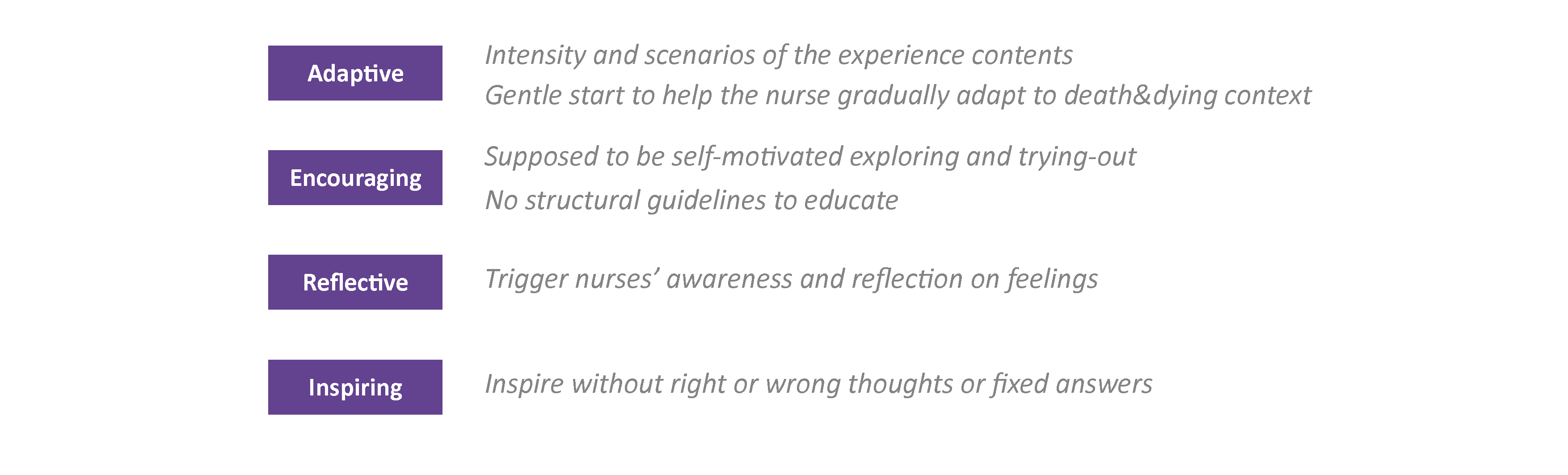
“How to create experience journeys of interacting with patient&family in VR, where nurses are able to become emotional and spiritual prepared to provide palliative terminal care for dying patients in Maasstad Hospital, and be able to help patients&family recognize and cope with emotional&spiritual issues.”
The reason that choosing to focus on emotional and spiritual capability is because that:
︎ Emotional and spiritual needs and capability of the formal caregivers in palliative care, like nurses, are rarely discussed and addressed compared with practical and professional skills and capability. However, the nurses in the medical system should also be perceived as a person like patients to be taken care of, not only to be perceived as a functional tool.
︎ The acquire of emotional and spiritual capability can, in turn, contribute to better professional skill gaining on palliative care, which gives the nurses the feeling of security and confidence to behave, practuce skills, and interact with patients and their loved ones.
Value of VR:
︎ No effects on real patients and families
︎ VR learners are four times faster than learning in the traditional way (PwC VR soft skill training efficacy study, 2020)
︎ Flexible (anytime and anywhere)
︎ Maasstad Hospital is already having collaboration with VR companies, which shows potential development and launching opportunities.
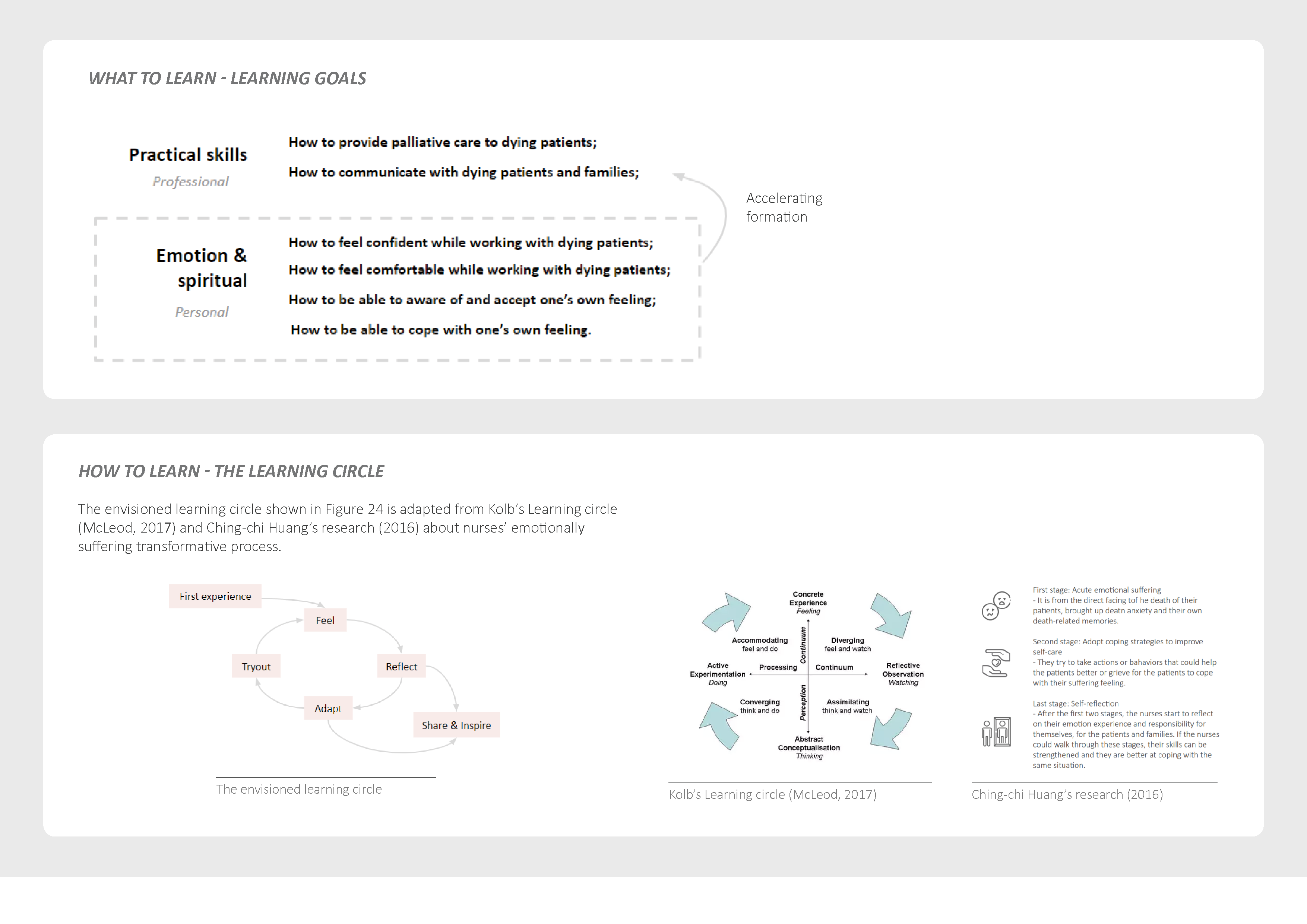
Remark: The aim of learining
on emotional and spiritual aspects is not to make nurses to be
comfortable with death and dying. We all have the right to have our own visions and
beliefs on death and dying.
The design hopes to support
nurse to be able to be aware of what they feel as part of themselves and achieve to
know how they can get along with their nevigate feelings. The design also aims to
inspire the nurses that they are making a difference for the patients and families.
Stakeholders:

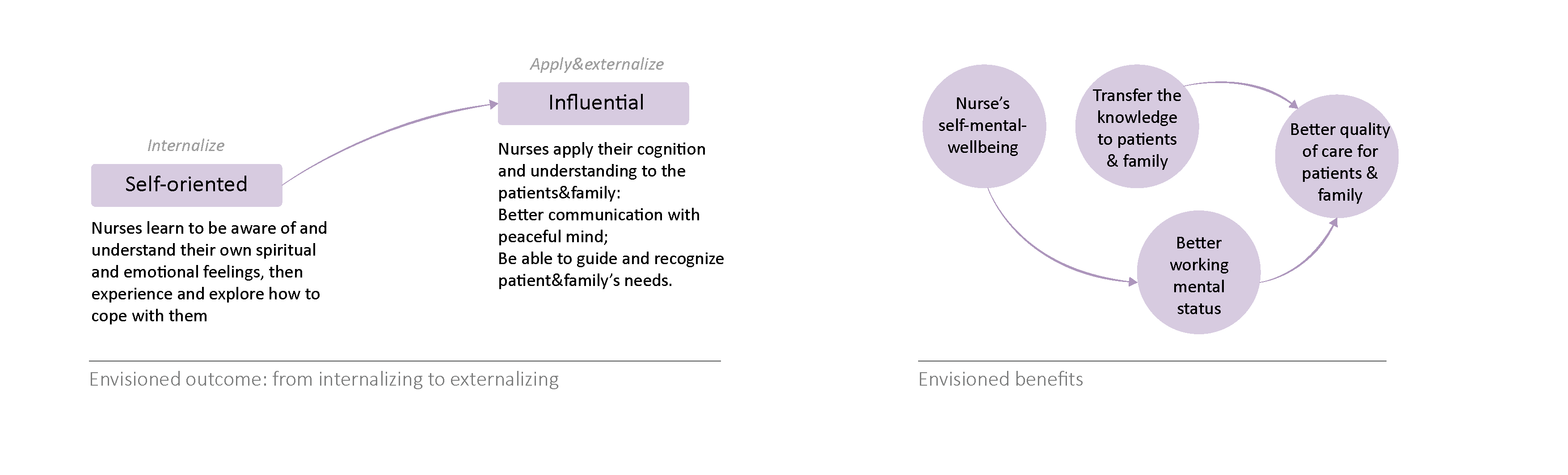
Envisioned outcome:
By creating the learning and experience journey in a VR application, the nurses are expected to gradually learn how to perceive and cope with their emotional and spiritual needs and burdens. From there, they are able to externalize their sensitivity and skills on influencing patients and their loved ones, including understand and recognize patient&- family’s emotional&spiritual needs, as well as guide and provide support on those needs.
Interaction vision:
3. Ideation
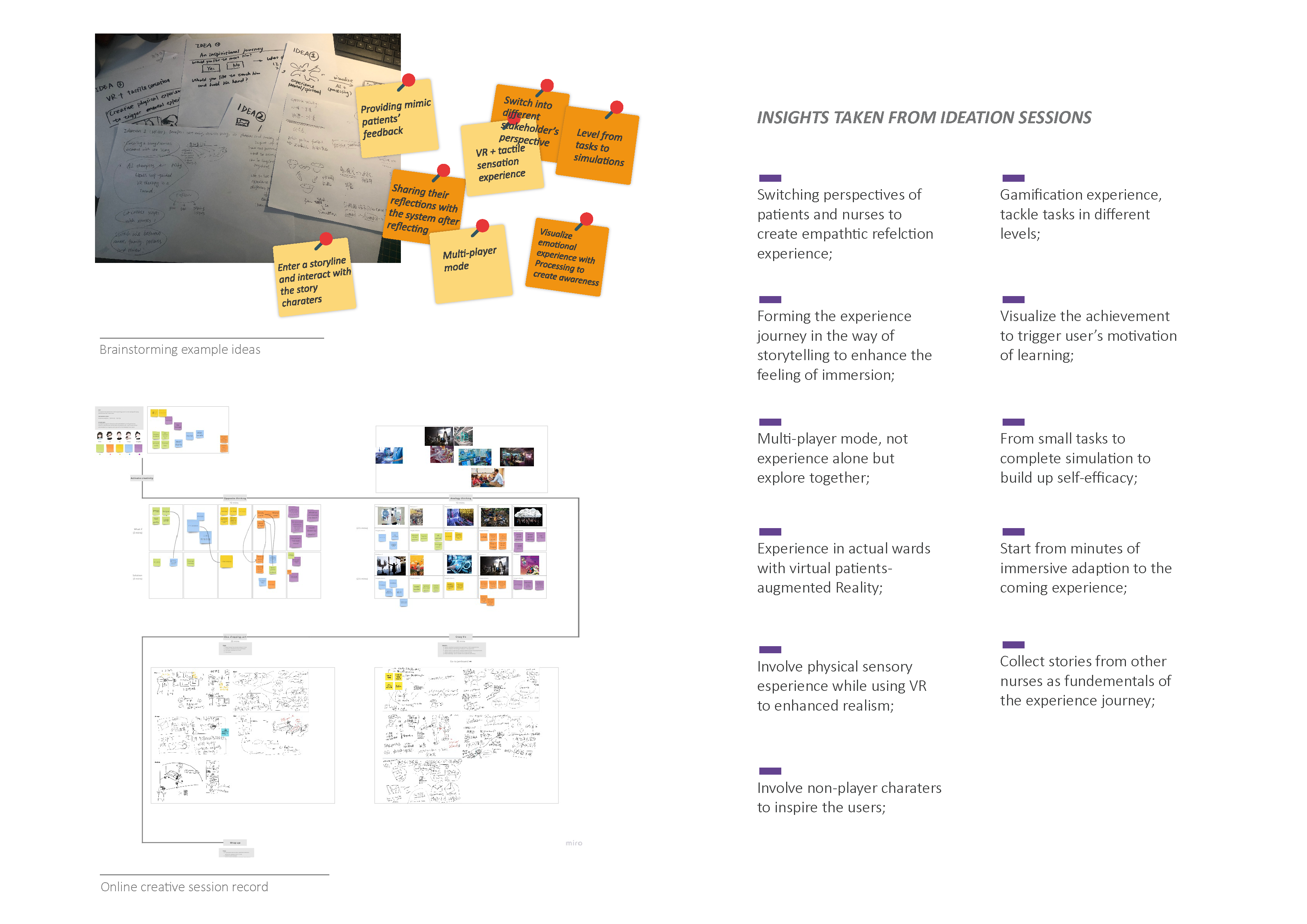
To develop the brief of design into a concrete solution, design ideation sessions are conducted at this phase.![]()
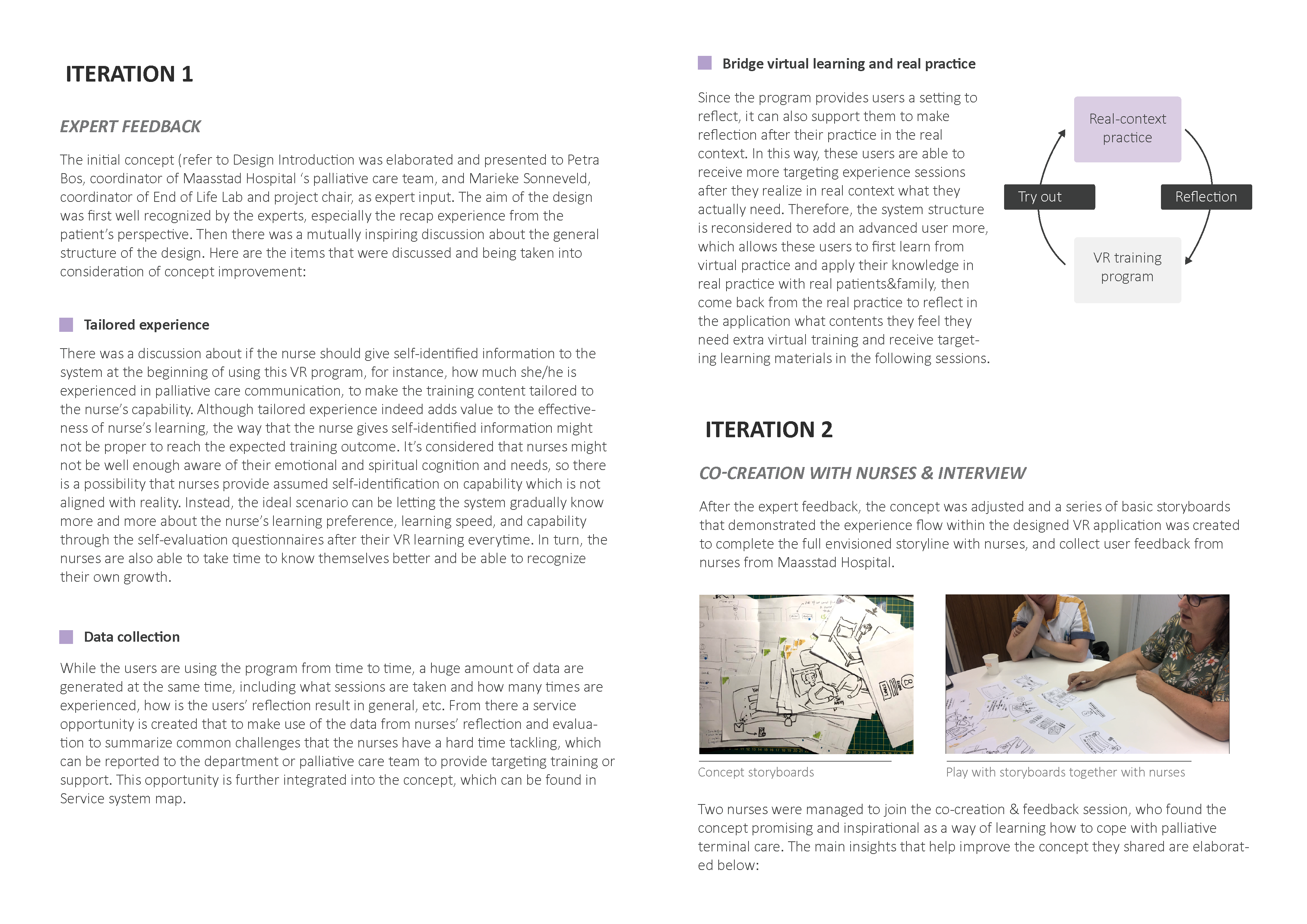
The creative ideation session is planned for absorbing fresh ideas and new perspectives to look at the design goal from different mindsets. This session was also expected to invite the nurses from Maasstad Hospital as a designer- stakeholders co-creation session. However, due to the special circumstance of pandemic with limited access to the hospital and nurses, the plan was adjusted to only have student designers from different design disciplines to inspire and challenge each other, and involve nurses at a later stage when iterating on the initial concept.
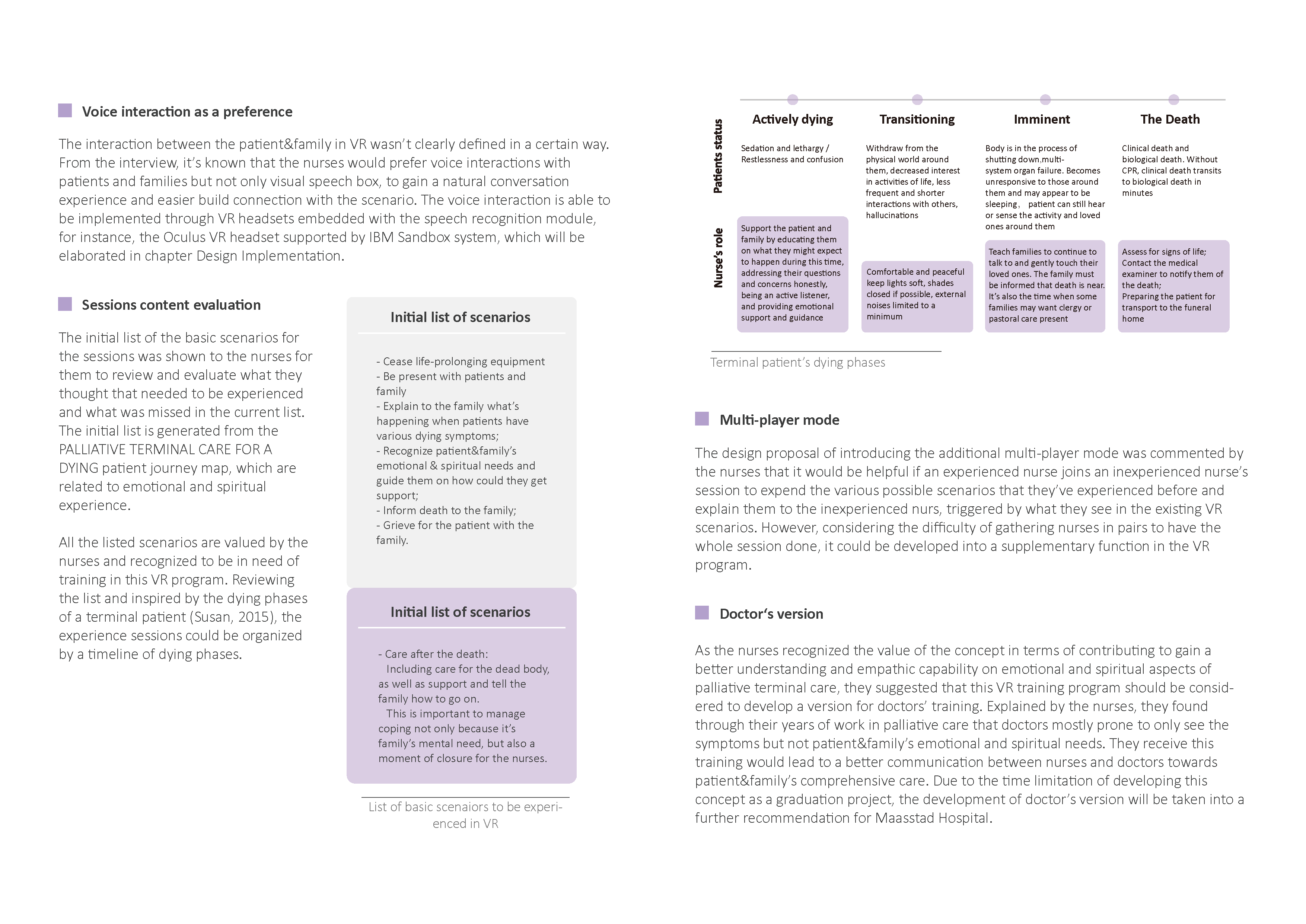
In this session, all the participants reviewed the design goal together and tried to interpret it from different scenarios, broadening the solution possibiliteis. The outcome of the creative session are several concept sketches of envisioned journeys of the training experience. These sketches inspire the generatoin of the initial concept with a complete user experience journey in VR. The setup of the session and outcomes of each step can be found Here︎︎︎.
4. Conceptualization
To develop the brief of design into a concrete solution, design ideation sessions are conducted at this phase.
The creative ideation session is planned for absorbing fresh ideas and new perspectives to look at the design goal from different mindsets. This session was also expected to invite the nurses from Maasstad Hospital as a designer- stakeholders co-creation session. However, due to the special circumstance of pandemic with limited access to the hospital and nurses, the plan was adjusted to only have student designers from different design disciplines to inspire and challenge each other, and involve nurses at a later stage when iterating on the initial concept.
In this session, all the participants reviewed the design goal together and tried to interpret it from different scenarios, broadening the solution possibiliteis. The outcome of the creative session are several concept sketches of envisioned journeys of the training experience. These sketches inspire the generatoin of the initial concept with a complete user experience journey in VR. The setup of the session and outcomes of each step can be found Here︎︎︎.
4. Conceptualization
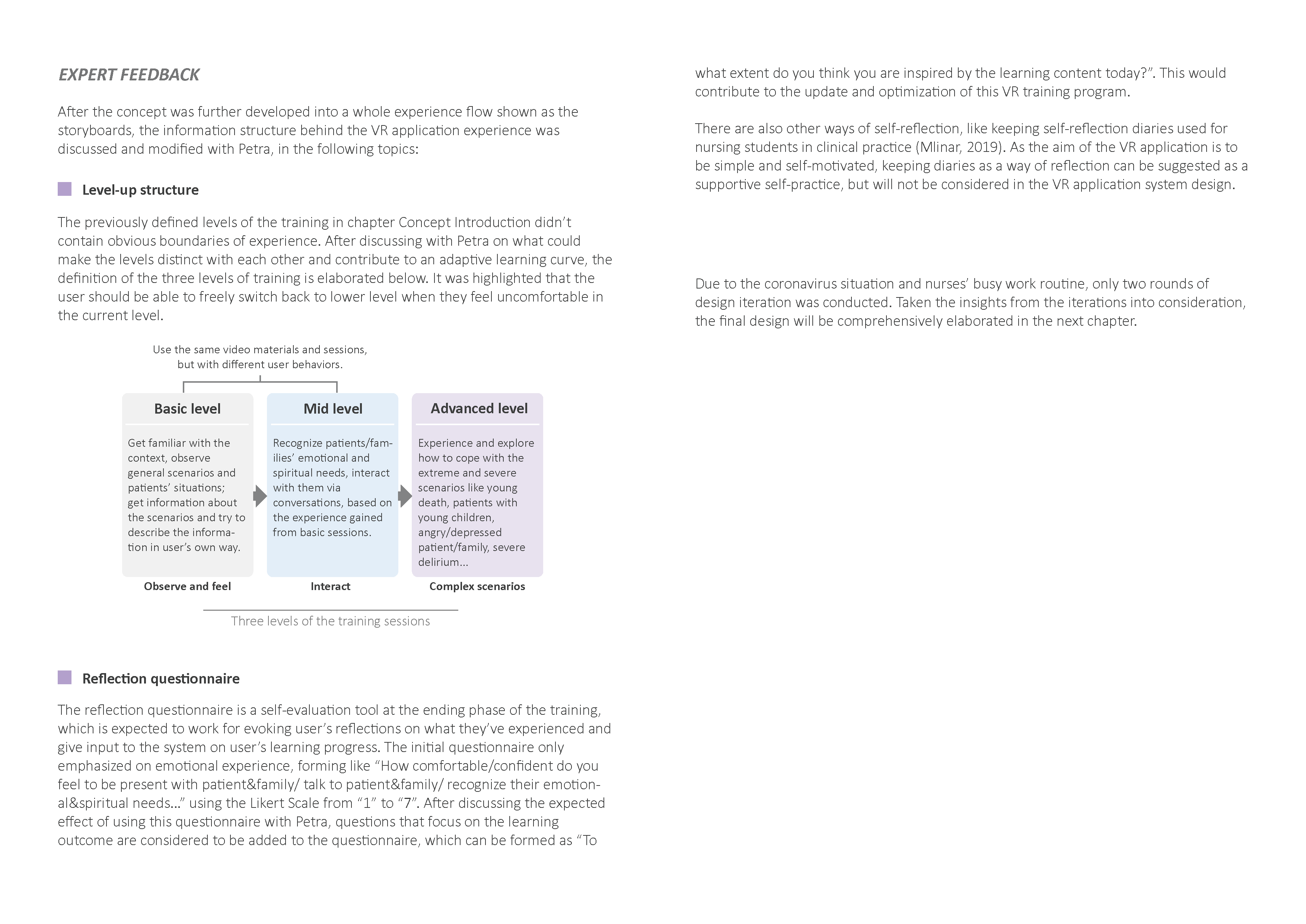
5. Iterations
6. Final design elaboration
User and stakeholders:

Interface and userflow:
Design implementation:
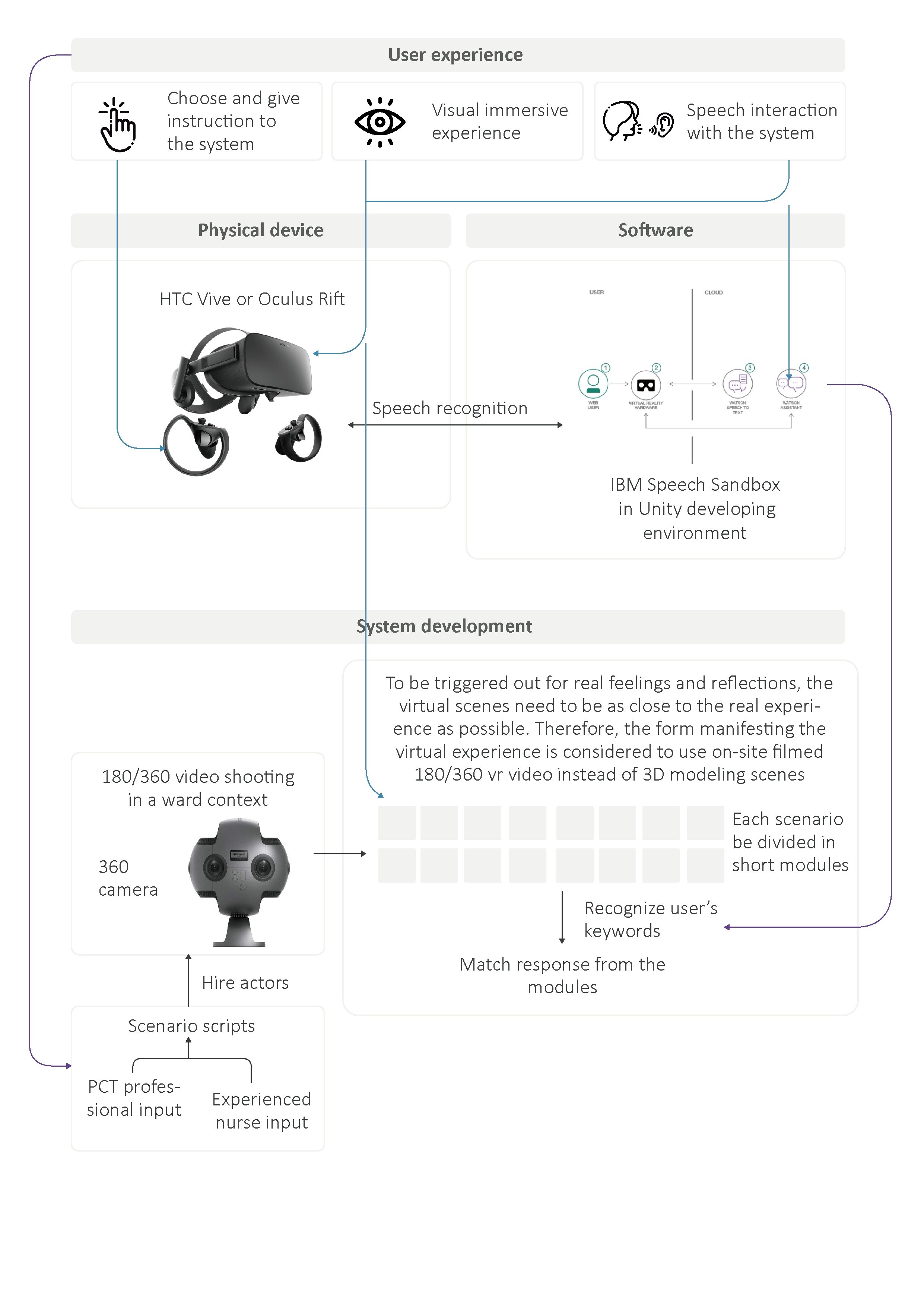
To be triggered out for real feelings and reflections, the virtual scenes need to be as close to the real experience as possible. Therefore, the form manifesting the virtual experience is considered to use on-site filmed 180/360 vr video instead of 3D modeling scenes use in most of the current nurse training VR applications.
Known from Maasstad Hospital, there is an organization Lotus Nederland which provides professional trained actors/actresses on medical training, who are able to reproduce the patients’ realistic status and reactions for care providers to practice. To create a more realistic experience in this VR application for the nurses, it can be considered to hire the actors/actresses from Lotus Nederland for the scenario filming.
Demo making
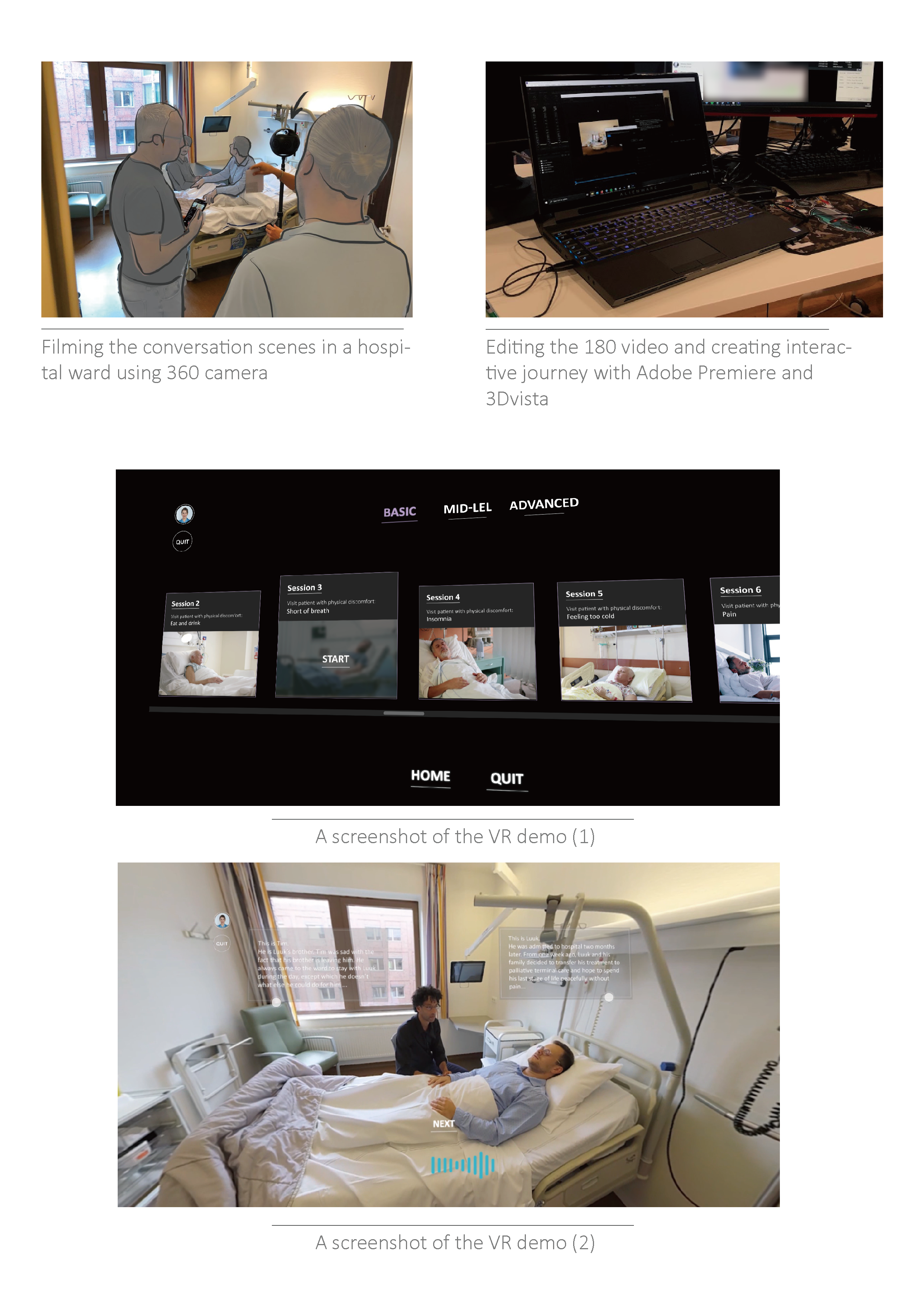
To gain valuable and relatively accurate feedback of the design from the users, an interactive demo which can be experienced with VR headsets is created, technically supported by VR Zone, TU Delft. The demo includes a basic user journey, that is close to the envisioned design outcome, from a beginning to the end of a single time of use, consisting of two scenarios which are interaction with a patient and interaction with a patient’s family. Due to the time and technical limitations, the speech interaction isn’t implemented in this demo but only simulated by the recorded users’ voice.
7. Design evaluation
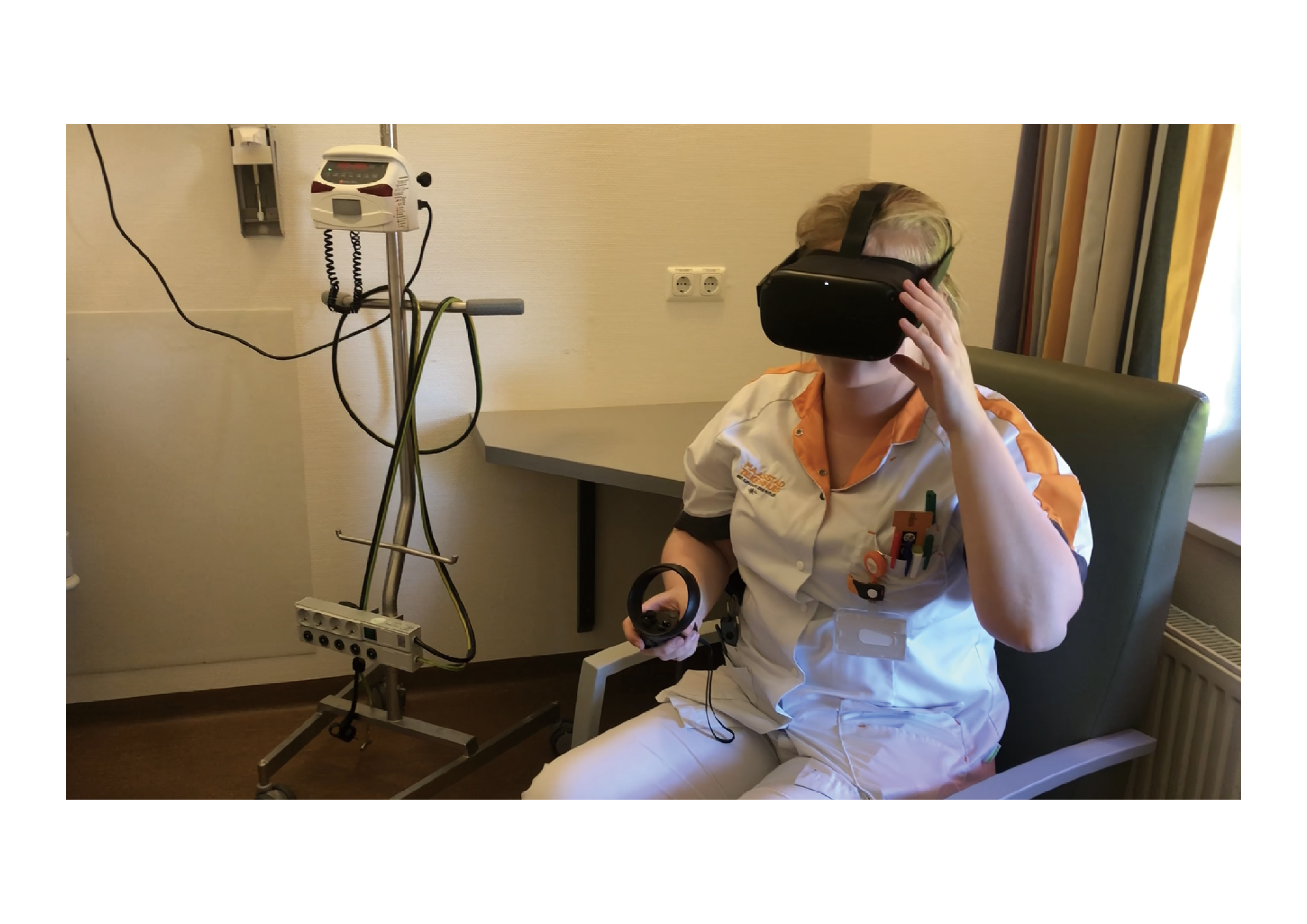
As general, from 1 to 10 scores, the nurse gave an 8 for the final design outcome as it’s a new perspective for them to get trained and adapted to palliative care practice, and she believed that the design would have a great contribution to young/inexperienced nurses’ palliative care education. In the figure below, the evaluation of how the design has matched with the interaction vision is elaborated.

Based on the final evaluation result, the design is perceived as a good start of this proposed VR training application, which possesses potentials to provide the inexperienced nurses or even other medical professionals with a safe environment to think about the topic of palliative terminal care, learn to cope with their own feelings, explore and make mistakes, and be eventually more comfortable and confident to look after dying patients and their family members. However, since the design mainly focuses on the training program structure and the experience journey, more opportunities and details of the interaction design still need to be developed and tested if the application is expected to be launched.
Generally, the final outcome of this project introduces a potential solution for Maasstad’s nurses who don't receive specialized palliative care education or training to get themselves feel more prepared for providing palliative terminal care to patients and families, ensuring nurses’ own mental well-being as well as better care quality. If it is further developed and assessed as effective, it can be perceived as an intervention that bridges the current situation and the envisioned situation when palliative care education becomes available or compulsory for all care providers. However, when the envisioned situation comes, this solution is not necessary to be conflict or overlapped with the mature palliative care education & training system, but can be part of it, because of the different perspective to conquer the challenge of palliative care practice and an important supplementary to the knowledge gained from instructions and guidelines.
“ I talked with other colleagues in palliative care domain about this concept
and found they are all enthusiastic about it for its freshness and looking at
the problem from a different perspective, it’s not only writing a model or
playing something, but getting the nurses into real situations but in a safer
environment where they can make mistakes. We’d love to see the project
being developed as soon as possible and involve more beginning nurses to
share their opinion on it, and spread the idea to other departments...”
----- Priscilla (Palliative care coordinator, Maasstad Hospital)
----- Priscilla (Palliative care coordinator, Maasstad Hospital)